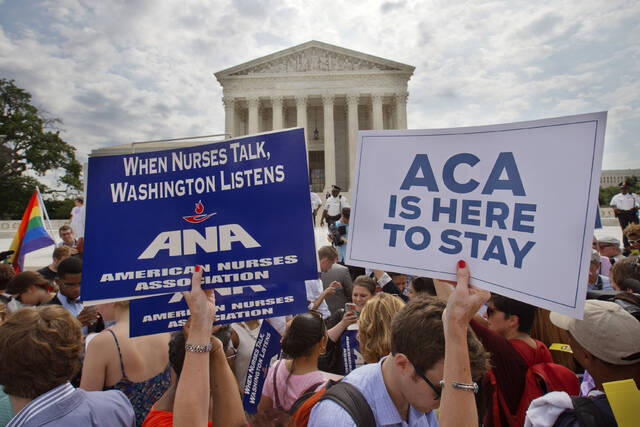
WASHINGTON — The Supreme Court preserved a key part of the Affordable Care Act’s preventive health care coverage requirements on Friday, rejecting a challenge from Christian employers to the provision that affects some 150 million Americans.
The 6-3 ruling comes in a lawsuit over how the government decides which health care medications and services must be fully covered by private insurance under former President Barack Obama’s signature law, often referred to as Obamacare.
The plaintiffs said the process is unconstitutional because a volunteer board of medical experts tasked with recommending which services are covered is not Senate approved.
President Donald Trump’s administration defended the mandate before the court, though the Republican president has been a critic of his Democratic predecessor’s law. The Justice Department said board members don’t need Senate approval because they can be removed by the health and human services secretary.
Medications and services that could have been affected include statins to lower cholesterol, lung cancer screenings, HIV-prevention drugs and medication to lower the chance of breast cancer for women.
The case came before the Supreme Court after an appeals court struck down some preventive care coverage requirements. The U.S. 5th Circuit Court of Appeals sided with the Christian employers and Texas residents who argued they can’t be forced to provide full insurance coverage for things like medication to prevent HIV and some cancer screenings.
Well-known conservative attorney Jonathan Mitchell, who represented Trump before the high court in a dispute about whether he could appear on the 2024 ballot, argued the case.
The appeals court found that coverage requirements were unconstitutional because they came from a body — the United States Preventive Services Task Force — whose members were not nominated by the president and confirmed by the Senate.
A 2023 analysis prepared by the nonprofit KFF found that ruling would still allow full-coverage requirements for some services, including mammography and cervical cancer screening.